Patients on complex specialty therapies always have lots of questions. Lately they have been asking lots of questions about the Covid-19 vaccines and whether they are safe for given that they many are immune compromised. The good news… as detailed below, currently approved vaccines are safe for MS patients. But…..
We recently sent a report on this question pertaining to patients on inflammatory therapies. It included detail on the timing of vaccine administration and temporary pausing the specialty therapy. Today we are spotlighting MS patients. Their Disease Modifying Therapies (DMTs) can diminish immune response to the vaccines since they are designed to suppress the body’s immune system.
So, how long after the DMT is paused is it advised to receive vaccine and how long after the vaccine is administered is it advised before restarting or starting each DMT? See the list of drugs below.
Yes, there will be a quiz!
A specialty pharmacy usually has detailed clinical protocols for all its therapies. The vaccines present a great opportunity for targeted protocols…. by therapy. Manufacturers should be able to provide this information, so you don’t need to do all the heavy lifting.
National MS Society Offers Guidelines for Timing of COVID-19 Vaccines
March 29, 2021 — Vaccines for COVID-19 are safe and strongly recommended for all patients with multiple sclerosis (MS), according to new guidance from the National MS Society.
The guidance urges all MS patients to get vaccinated as soon as possible. Those in high-risk groups whether due to having progressive MS or any other reason “are especially encouraged to get vaccinated as soon as it becomes available,” the guidance states.
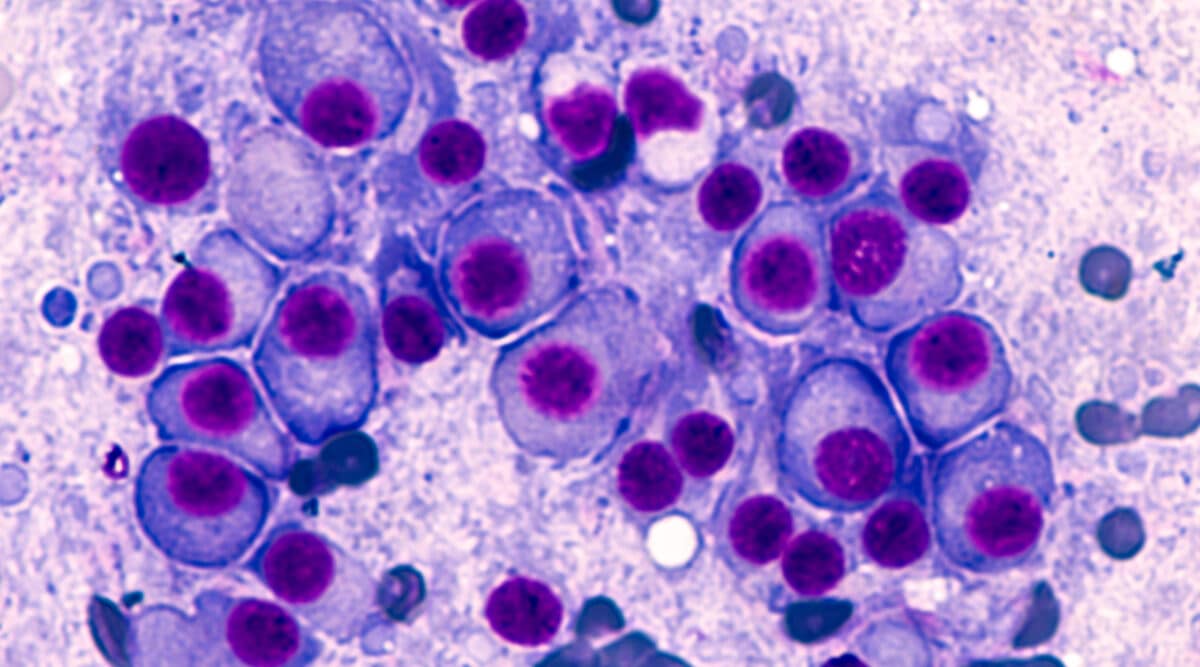
“A question that does come up, though, is whether to consider timing the vaccination relative to some of the disease-modifying therapies (DMTs) to maximize the immune response to the vaccine,” Dr. Bar-Or said. The guidance notes that some DMTs might diminish patients’ immune response to the vaccines, precisely because they are designed to tamp down the body’s immune system.
Specialists should consider how long after the DMT they should start vaccine and how long after the vaccine they might wait prior to restarting or starting DMT, Dr. Bar-Or said.
For some DMTs, it is enough to wait two weeks, for others it would be probably better to wait four weeks between completed vaccines and (re)starting DMT, he said, adding, “This may warrant a case-by-case discussion between the person living with MS and their provider, since settings and circumstances can differ.”
For example, Dr. Bar-Or said, a patient who is prescribed ocrelizumab for active relapsing MS, who is younger, not disabled and without comorbidities, could get the COVID-19 vaccine when it is offered, or plan to complete the vaccination several weeks prior to the next regularly scheduled ocrelizumab infusion.
“In contrast,” he said, “a patient prescribed ocrelizumab for primary progressive MS—who may also be older, more disabled and have one or more co-morbidities, and therefore at higher risk of severe COVID-19,—is unlikely to lose much ground if his ocrelizumab infusion is delayed by up to two or three months, potentially allowing for more robust vaccine response. That’s why it’s important for patients to discuss any timing adjustments with their neurologist.”
Guidance for Specific MS Drugs
No adjustment in timing is necessary, the guidance states, for MS patients taking beta interferons, any glatiramer acetate, teriflunomide, monomethyl fumarate generic dimethyl fumarate, diroximel fumarate, or natalizumab.
For patients whose MS is stable, neurologists and patients can consider the following adjustments in the administration of the DMT to maximize the vaccine’s effectiveness. Such scheduling is not always possible, however, and the guidance emphasizes that getting the vaccine when it becomes available may be more important than coordinating timing of the vaccine with the DMT dose.
- Sphingosine 1 phosphate receptor modulators: If a patient is about to start taking one of these medicines for the first time, they and their physician can consider waiting two to four weeks or more after getting fully vaccinated. If they are already on these therapies, they should continue taking them as prescribed and get vaccinated as soon as the vaccine is available to them.
- Alemtuzumab: If a patient is about to start alemtuzumab for the first time, they and their physician should consider waiting four weeks or more after being fully vaccinated. If they are already taking alemtuzumab, they should consider getting vaccinated 24 weeks or more after the last alemtuzumab dose. If they are due for their next treatment course, when possible, they should resume the therapy four weeks or more after getting fully vaccinated.
- Oral cladribine: If a patient is about to start cladribine, they and their physician should discuss waiting two to four weeks after getting fully vaccinated. If they are already taking cladribine, the currently available limited data does not suggest that timing of the vaccine in relation to the dosing is likely to make a significant difference in vaccine response. If they are due for their next treatment course, when possible, they should resume cladribine two to four weeks after getting fully vaccinated.
- Anti-CD20 monoclonal infusions (ocrelizumab, rituximab, and biosimilars): Patients who are about to start infusions of these therapies should discuss with their neurologist if it would be safe to wait two to four weeks or more after getting fully vaccinated. If they are already taking ocrelizumab or rituximab, they can consider getting vaccinated 12 weeks or more after the last DMT dose. When possible, ocrelizumab or rituximab should be resumed four weeks or more after getting fully vaccinated.
- Ofatumumab: Patients about to start ofatumumab for the first time should consider, in consultation with their physician, waiting two to four weeks or more after getting fully vaccinated. If they are already taking ofatumumab there is no data to currently guide timing of the vaccine in relation to their last DMT injection. When possible, the guidance recommends, patients should resume these injections two to four weeks after getting fully vaccinated.
- High-dose steroids: Patients and physicians should consider waiting at least three to five days after the last dose of steroids to begin the vaccine injection(s).