The FDA approval of the new therapy for Alzheimer’s is like no other in recent memory and has generated a firestorm reaction from both supporters and opponents.
Public Comments include…..
Cons: “The proof of efficacy just isn’t there!” and “The clinical benefit was barely detectable!”
Pros: “Finally my mother has hope.” and “We now have something to offer our patients who have been waiting years for a new therapy.”
The new once-monthly, infused drug is Aduhelm (aducanumab) from Biogen. It is easy to understand desperate patients and families wanting hope, but, members of the FDA advisory panel were not convinced. None voted to support the approval and three members have since resigned in protest. The FDA did mandate a post -launch clinical trial, however. Biogen, and its partner Esai, now have until 2029 to complete that trial to confirm the drug’s benefits for Alzheimer’s patients. That did not impress the advisory panel members and a very large number of medical experts nationally.
At the crux of the matter, Aduhelm hasn’t been shown to help slow the brain-destroying disease. A reassessment of data from only one trial arm showed statistically small slowing of declines in cognition and day-to-day function. A Biogen statement suggested that even for those for whom it has little or no effect, it offers that hope consumers are demanding. “Hope is a good thing.” That argument seems to have saved the day for Biogen.
Why such pressure to offer hope?
The last therapy approved for Alzheimer’s was 18 years ago. Alzheimer’s gradually attacks areas of the brain needed for memory, reasoning, communication and basic daily tasks. It’s the most common cause of dementia and the sixth leading cause of death in this country. After diagnosis, senior patients only live four to eight years, on average. So, the approval of a new any drug is a spark of hope.
But, that hope comes at a cost.
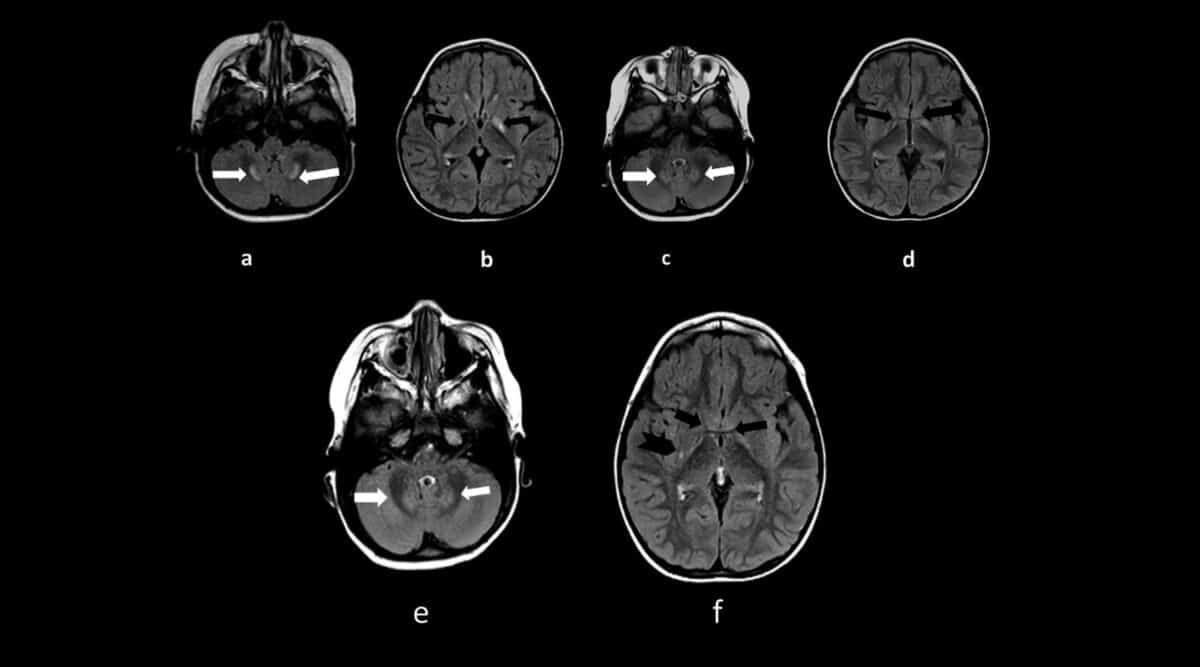
First, about 35 percent of all trial patients experienced painful brain swelling and, in some cases, bleeding in the brain.
Second, the therapy will hit the market with a price tag of $56,000 annually. Much of the media coverage in recent days has speculated about how payers will cover the drug. For example, Medicare Part B is expected to cost patients upwards of $11,000 annually out-of-pocket.
Biogen estimates that about 1.4 million people would be eligible to be treated by Aduhelm. Let’s assume that only 5% of these patients receive Aduhelm therapy. In that case, Biogen sales could hit upwards of $4 billion annually! According to Biogen about 900 U.S. medical facilities are ready to begin prescribing the drug, with many more expected.
Biogen did not announce distribution details. However, we are already hearing that a handful of specialty pharmacies will be integral to channel access. If a limited distribution program (direct to provider) is adopted, those specialty pharmacies may be realizing a huge revenue tsunami in coming months.
FDA Grants Accelerated Approval for Alzheimer’s Drug
June 07, 2021 — Today, the U.S. Food and Drug Administration approved Aduhelm (aducanumab) for the treatment of Alzheimer’s, a debilitating disease affecting 6.2 million Americans. Aduhelm was approved using the accelerated approval pathway, which can be used for a drug for a serious or life-threatening illness that provides a meaningful therapeutic advantage over existing treatments. Accelerated approval can be based on the drug’s effect on a surrogate endpoint that is reasonably likely to predict a clinical benefit to patients, with a required post-approval trial to verify that the drug provides the expected clinical benefit.
“Alzheimer’s disease is a devastating illness that can have a profound impact on the lives of people diagnosed with the disease as well as their loved ones,” said Patrizia Cavazzoni, M.D., director of the FDA’s Center for Drug Evaluation and Research. “Currently available therapies only treat symptoms of the disease; this treatment option is the first therapy to target and affect the underlying disease process of Alzheimer’s. As we have learned from the fight against cancer, the accelerated approval pathway can bring therapies to patients faster while spurring more research and innovation.”
Alzheimer’s is an irreversible, progressive brain disorder that slowly destroys memory and thinking skills, and eventually, the ability to carry out simple tasks. While the specific causes of Alzheimer’s disease are not fully known, it is characterized by changes in the brain—including amyloid plaques and neurofibrillary, or tau, tangles—that result in loss of neurons and their connections. These changes affect a person’s ability to remember and think.
Aduhelm represents a first-of-its-kind treatment approved for Alzheimer’s disease. It is the first new treatment approved for Alzheimer’s since 2003 and is the first therapy that targets the fundamental pathophysiology of the disease.
Researchers evaluated Aduhelm’s efficacy in three separate studies representing a total of 3,482 patients. The studies consisted of double-blind, randomized, placebo-controlled dose-ranging studies in patients with Alzheimer’s disease. Patients receiving the treatment had significant dose-and time-dependent reduction of amyloid beta plaque, while patients in the control arm of the studies had no reduction of amyloid beta plaque.
These results support the accelerated approval of Aduhelm, which is based on the surrogate endpoint of reduction of amyloid beta plaque in the brain—a hallmark of Alzheimer’s disease. Amyloid beta plaque was quantified using positron emission tomography (PET) imaging to estimate the brain levels of amyloid beta plaque in a composite of brain regions expected to be widely affected by Alzheimer’s disease pathology compared to a brain region expected to be spared of such pathology.
The prescribing information for Aduhelm includes a warning for amyloid-related imaging abnormalities (ARIA), which most commonly presents as temporary swelling in areas of the brain that usually resolves over time and does not cause symptoms, though some people may have symptoms such as headache, confusion, dizziness, vision changes, or nausea. Another warning for Aduhelm is for a risk of hypersensitivity reactions, including angioedema and urticaria. The most common side effects of Aduhelm were ARIA, headache, fall, diarrhea, and confusion/delirium/altered mental status/disorientation.
Under the accelerated approval provisions, which provide patients suffering from the disease earlier access to the treatment, the FDA is requiring the company, Biogen, to conduct a new randomized, controlled clinical trial to verify the drug’s clinical benefit. If the trial fails to verify clinical benefit, the FDA may initiate proceedings to withdraw approval of the drug.
Aduhelm was granted Fast Track designation, which seeks to expedite the development and review of drugs that are intended to treat serious conditions where initial evidence showed the potential to address an unmet medical need.
Aduhelm is made by Biogen of Cambridge, Massachusetts.